As labor and supply costs continue to rise and reimbursement structures struggle to keep pace, healthcare organizations are searching every corner for cost-saving measures to maintain margin and profitability. The operating room (OR), which often generates 60–65% of patient revenues at an average hospital, also comes with substantial cost. Maximizing OR efficiency is a key opportunity for healthcare organizations to minimize costs and improve margins.
Considering labor hours, equipment, supply costs, and general overhead, the cost of one minute of OR time can range from $50 to $150. At this rate, even slight delays in throughput can translate to significant costs (or savings opportunities) when annualized. And, as OR managers know well, if the first case goes off the blocks late, there is a cascading effect throughout the day. That late start leads to additional delays, stress on staff to make up for lost time, and unhappy providers and patients. For this reason, first case on-time starts (FCOTs) are a core measure of OR efficiency and commonly tracked measure among hospital administrators. High-performing organizations strive for a FCOT rate of 90% or greater.
Falling below the industry standard of 90% can have significant cost implications. Consider, for example, a facility that has a 50% FCOT rate for a 10-room OR that starts on average 15 minutes late. Achieving the industry standard of 90% would create an annualized impact of $1.56 million at $100/minute/OR. If your organization isn’t tracking FCOTs, it’s likely you have a high percentage of canceled or delayed cases, frustrated staff, as well as large overtime spend that is eating into your bottom line.
A simple, but powerful method to optimize your OR schedule for FCOTs that meet the industry standard of 90% or greater is to implement a daily multidisciplinary OR planning huddle. Facilitated by the OR board runners, these huddles typically occur in the afternoon with the goal to review the morning cases to find out what went well, what did not, and how the team can better prepare for tomorrow.
They are intended to be brief calls, with the most efficient huddles lasting roughly 15 minutes. In that time, the team reviews the following day’s lineup and ensures all stakeholders are aware of any concerns that may lead to a delay or cancellation. But the huddle goes beyond information sharing. The intended outcome of each huddle is to adjust the following day’s lineup whenever necessary to optimize for FCOTs; that is, to ensure first cases are clean and ready to go.
Clean cases are those in which:
- Financial and medical clearances are obtained.
- Pre-admission testing processes are complete.
- All necessary test results are in and the anesthesia plan is reviewed.
- Preference cards are attached and ready to be picked.
- Vendor trays are in house with enough time to sterilize.
- Any safety concerns are known, communicated, and addressed.
Three considerations for a successful multidisciplinary huddle
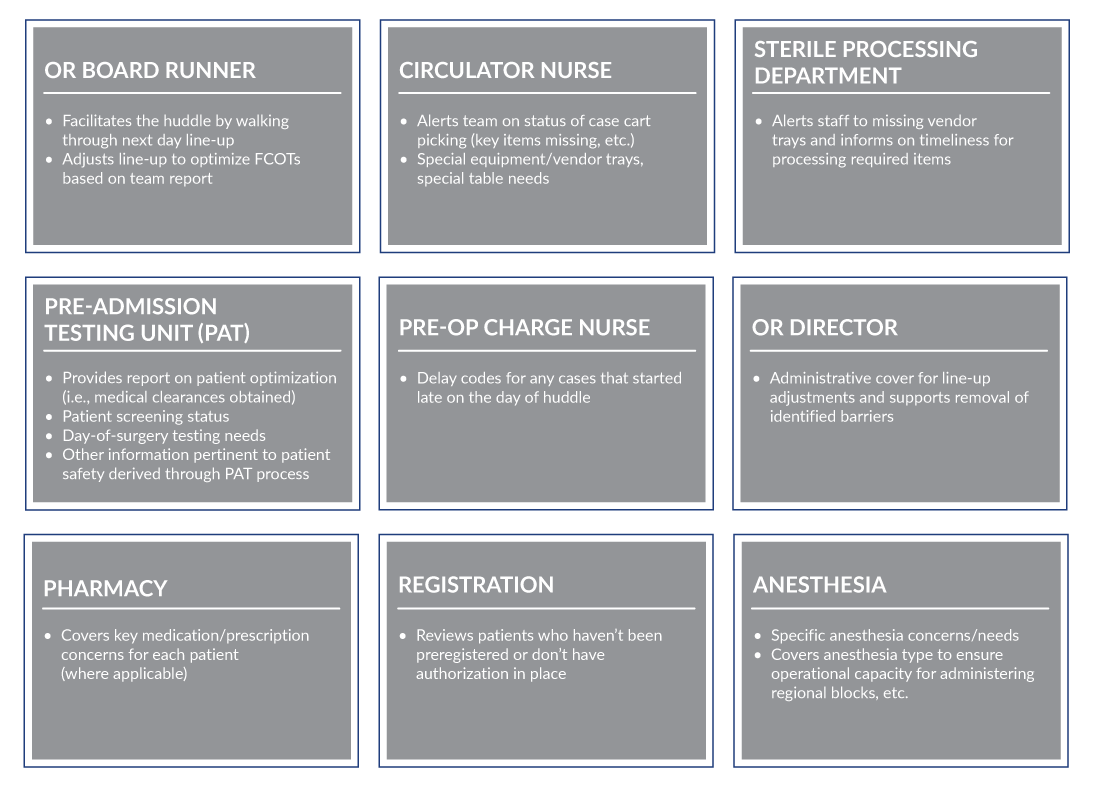
- Finding the right people: Take time to review your OR value stream and pull together the key stakeholders involved in getting a patient to an on-time surgery. The exact composition of personnel differs slightly for each organization, but the list below is a good starting point.
- Where and when to meet for huddle: It’s critical to have all team members present and ready to report for each huddle. For huddles that take place in person, choose a place where everyone can gather outside the RED line. This allows representatives from nonclinical areas to join and makes it easier for everyone to attend the huddle on-time. Virtual formats can work well but require extra vigilance in preparation and facilitation to ensure the team’s full attention. The huddle should occur before the pre-op charge nurse leaves for the day, but early enough to ensure adequate time to contact physician offices and address any potential issues before they close. Many hospitals choose a time around 1:00 p.m. for these reasons.
- How to measure progress: “Tracking and posting” FCOT data is a crucial factor to the success of multidisciplinary huddles. Most electronic medical records have a perioperative dashboard (e.g., OR manager in Epic) that can be leveraged for this purpose. Metrics should be posted where your huddle meets or displayed during huddle for review as part of a virtual discussion. The team should set and track a daily goal for each metric and the actual numbers from the previous week to measure progress against. Recommended daily measures to track include:
- Number of scheduled cases.
- Number of add-on cases.
- Huddle attendance level.
- Number of rooms starting before 9 a.m.
- Today’s FCOTs percentage achieved.
- Number of same-day cancels
A common data gap to watch for is incomplete or nonstandard use of delay codes when FCOT delays occur. Well understood and consistent charting of delay codes by the perioperative staff is essential. This enables OR directors to strategically address barriers to meeting FCOT goals.
The potential payoff
So, what can you expect to gain from well-executed multidisciplinary OR huddles? If your organization is struggling with FCOTs and can’t reach the industry-standard 90% rate, a well-executed multidisciplinary planning huddle is a powerful tool to move the needle. The improvement can result in significant improvements in OR utilization and decreased overtime spend. Benefits also include substantial nonfinancial factors such as reduced staff stress and patient frustration from canceled or delayed cases.
Bottom line
Navigating operational improvement in multidisciplinary fields is challenging, and as with most process improvement projects, success rates rise when there’s a strong leadership focus and buy-in from the team. With OR facilities generating significant revenues and costs for health systems, implementing a multidisciplinary planning huddle to improve FCOT rates is a piece of “low-hanging fruit” that’s well worth the time and investment.





